Depression affects millions of Americans each year, yet many people suffering from this condition don’t receive the support they need. At Windansea Recovery, we understand that recognizing depression in someone you care about can be challenging. Symptoms may develop gradually, and many people struggling with depression become adept at hiding their pain from others. This guide will help you identify potential signs of depression in a loved one and provide guidance on how to approach this sensitive situation with compassion and understanding.
Understanding Depression
Before exploring specific signs, it’s important to understand that depression is more than just feeling sad or going through a temporary rough patch. Clinical depression (major depressive disorder) is a serious mental health condition that affects how a person thinks, feels, and functions in daily life. It’s a medical condition that can benefit significantly from proper treatment and support.
Depression can affect anyone regardless of age, gender, or background. It often emerges from a complex interaction of factors including:
- Biological and genetic predispositions
- Brain chemistry imbalances
- Hormonal changes
- Early childhood experiences and trauma
- Life transitions and major stressors
- Medical conditions and medications
- Substance use
Common Signs of Depression to Watch For
Depression manifests differently in each person, but there are several common signs that may indicate your loved one is struggling. Look for patterns and clusters of these symptoms, especially if they persist for more than two weeks:
Emotional Signs
- Persistent sadness or low mood that doesn’t seem to lift with positive events
- Increased irritability or a shorter temper than usual, particularly in men and adolescents
- Feelings of emptiness, hopelessness, or worthlessness sometimes expressed through comments about feeling like a burden
- Loss of interest or pleasure in previously enjoyed activities (anhedonia)
- Unexpected emotional reactions such as crying without an obvious trigger
- Expressions of guilt over minor matters or things beyond their control
- Talk of death or suicide, whether direct or indirect, which should always be taken seriously
Behavioral Changes
- Withdrawal from social activities and increasing isolation
- Declining performance at work or school
- Neglect of responsibilities or personal hygiene
- Changes in communication patterns, such as less frequent calls or texts
- Increased use of alcohol or substances as a potential self-medication
- Restlessness or lethargy in movement and activities
- Sleep disturbances – either sleeping too much or experiencing insomnia
- Changes in eating patterns resulting in significant weight loss or gain
Cognitive Signs
- Difficulty concentrating or making decisions
- Memory problems that weren’t previously present
- Slower thinking or speech than usual
- Negative thought patterns focused on failure, guilt, or worthlessness
- Expressing a bleak or hopeless view of the future
- Rumination on past mistakes or regrets
Physical Symptoms
- Persistent fatigue and lack of energy that isn’t relieved by rest
- Unexplained aches and pains without clear physical cause
- Headaches or digestive problems that don’t respond to treatment
- Moving or speaking more slowly than usual
- Psychomotor agitation (restless movements, inability to sit still)
Special Considerations for Different Populations
Depression in Men
Men may express depression differently than what’s typically expected. Watch for:
- Increased anger, irritability, or aggressiveness
- Risk-taking behavior
- Using work as an escape and becoming a “workaholic”
- Controlling, violent, or abusive behavior
- Greater focus on physical symptoms rather than emotional ones
- Difficulty meeting work, family, or other responsibilities
Depression in Adolescents and Young Adults
Young people may show depression through:
- Irritability and anger rather than sadness
- Extreme sensitivity to criticism
- Withdrawal from some, but not all social situations
- Vocal expressions of feeling misunderstood
- Poor performance in school
- High-risk behaviors and substance experimentation
- Excessive use of social media or gaming as escape mechanisms
Depression in Older Adults
Older individuals might experience depression as:
- Memory difficulties or personality changes that mimic dementia
- Physical aches and pains that dominate their concerns
- Less willingness to acknowledge feelings of sadness or grief
- Fixation on death or feeling they’ve lived long enough
- Neglect of personal care or medical regimens
When and How to Approach a Loved One About Depression
If you notice several signs of depression in someone you care about, consider these approaches for starting a compassionate conversation:
Choosing the Right Moment
- Find a private, comfortable setting without distractions
- Allow plenty of time without rushing the conversation
- Choose a moment when both of you are calm, not during an argument
- Consider a side-by-side activity (like walking) that may feel less confrontational than a face-to-face talk
Starting the Conversation
- Begin with “I” statements about your observations: “I’ve noticed that you seem to have less energy lately” rather than “You’re always so negative”
- Express genuine concern without judgment: “I care about you and have been worried”
- Be specific about behaviors you’ve noticed without interpreting them
- Ask open-ended questions and listen more than you speak
- Validate their feelings even if you don’t understand them
What to Avoid
- Don’t diagnose them or use clinical language that might feel labeling
- Avoid minimizing their feelings with phrases like “just snap out of it” or “we all feel sad sometimes”
- Don’t compare their situation to others who “have it worse”
- Resist the urge to offer solutions or “fix” their problems
- Never suggest that they’re just being dramatic or seeking attention
Offering Support
- Ask directly how you can help rather than assuming what they need
- Offer to help research treatment options or accompany them to an initial appointment
- Maintain consistent contact even when they might not reciprocate
- Set appropriate boundaries to protect your own mental health
When to Seek Professional Help
Certain situations indicate a need for immediate professional intervention:
- Expressions of suicidal thoughts or behaviors
- Inability to function in daily life or care for basic needs
- Psychotic symptoms such as hallucinations or delusions
- Severe withdrawal from life activities
- Co-occurring substance use that’s increasing in severity
If you’re concerned about immediate safety, call the National Suicide Prevention Lifeline at 988, go to your local emergency room, or call 911.
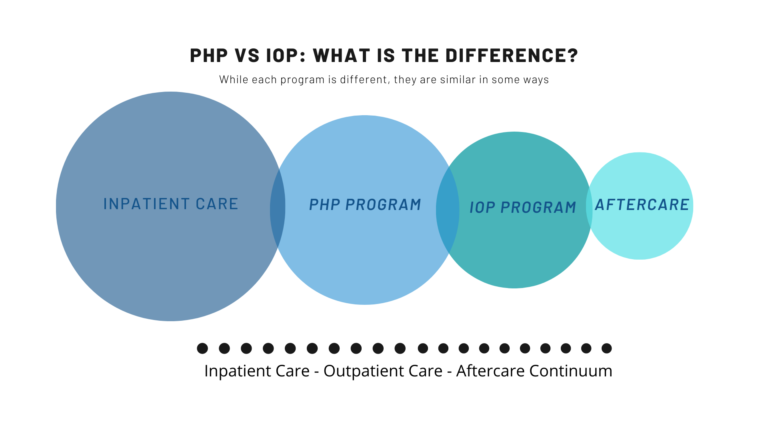
The Healing Journey at Windansea Recovery
At Windansea Recovery, we understand that depression rarely exists in isolation. Our integrated approach addresses not only the symptoms of depression but also co-occurring conditions like substance use disorders that often accompany depression.
Our La Jolla facility offers a tranquil coastal environment where healing can begin through:
- Comprehensive assessment to understand the full picture of an individual’s needs
- Evidence-based therapeutic approaches including CBT, DBT, and trauma-informed care
- Holistic modalities that support whole-person healing
- Community connection to combat the isolation depression often creates
- Family involvement to strengthen support systems
Supporting a Loved One Through Treatment
If your loved one begins treatment for depression, you can support their journey by:
- Educating yourself about depression and its treatment
- Attending family therapy sessions if invited
- Maintaining realistic expectations about recovery timelines
- Celebrating small improvements without putting pressure on progress
- Taking care of your own mental health and seeking support if needed
A Message of Hope
Depression, though serious, is one of the most treatable mental health conditions. With proper support and treatment, most people experience significant improvement in their symptoms and quality of life. Your compassionate attention to a loved one’s changing behaviors might be the first step toward their recovery journey.
If you notice signs of depression in someone you care about, reaching out with empathy can make a profound difference. And remember, professional support is available when needed. Contact Windansea Recovery at (619) 815-2555 or Contact Us Here to learn more about our approach to depression treatment and how we can help your loved one find their path to healing.
If you or someone you know is in crisis or experiencing thoughts of suicide, call or text 988 to reach the Suicide and Crisis Lifeline, available 24/7.